Let us show you how we
Identify, recover and even prevent overpayments
For all types of insurance payers
Let’s talk about Payer Challenges
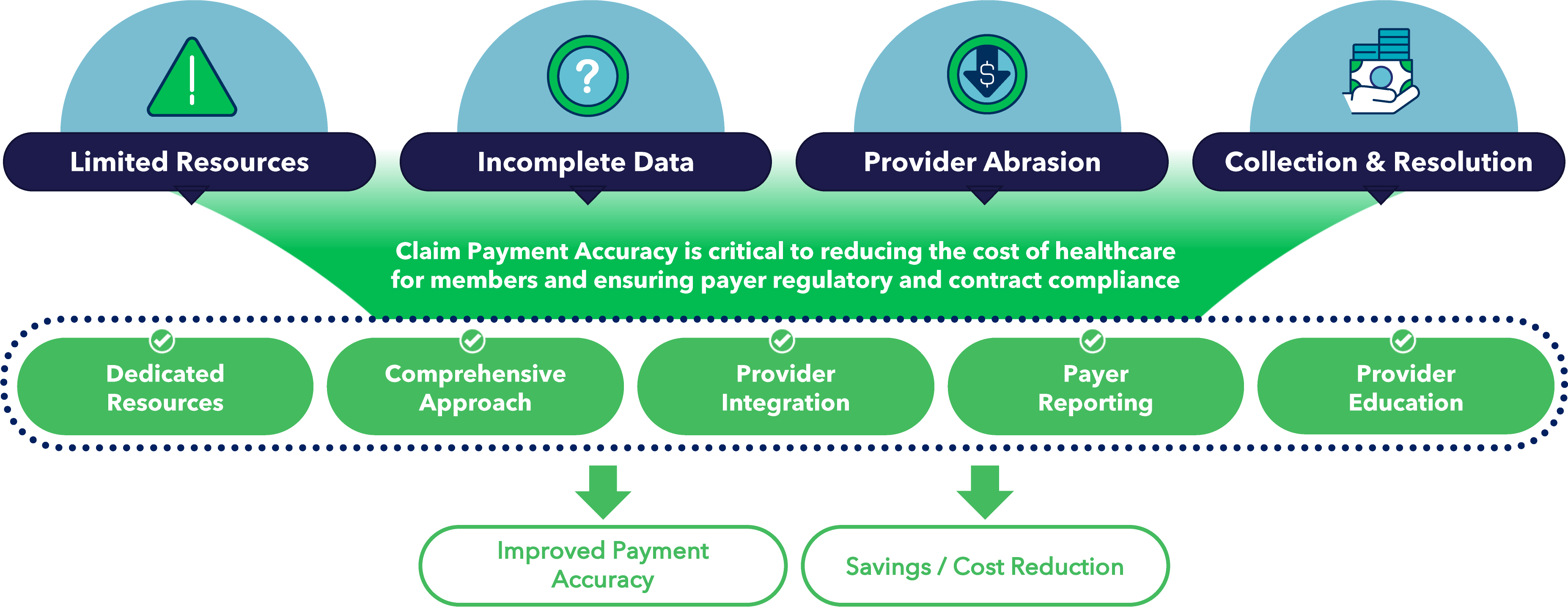



TREND Suite of Services
Expansive Array of Tech-enabled Services Driving Significant Value to Payers and Providers

Credit Balance & Overpayment Collections
CASE STUDY
Credit Balance

Plan Overview
State Medicaid Plan
Number of Members - 200K+
TREND reviews, validates and interacts directly with Provider on the Payer’s overpayment inventories that require approval for retraction or check recovery. TREND’S provider access and relationships expedite collections for our clients.

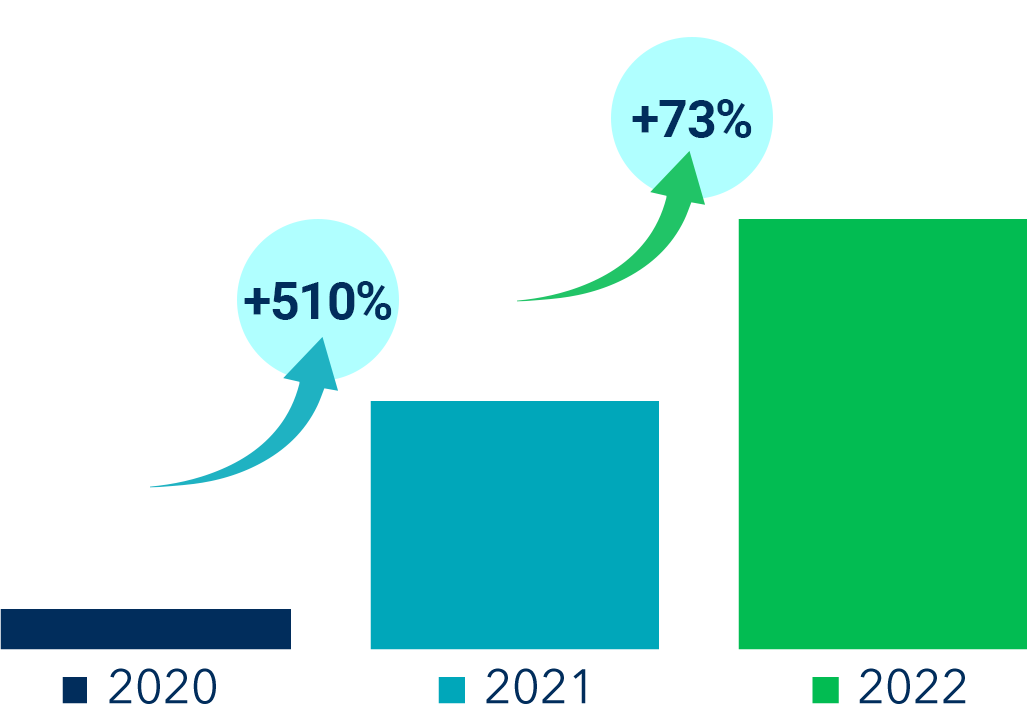
TREND History
Contracted payer for Credit Balance Service replacing another vendor state-wide in 2019

Key Value Drivers
Reduced payer refund denials by more than 50%
On-site representative reduces provider abrasion and helps create efficiency for Payer and Provider! Faster collection turnaround vs. standard mail/telephone collection process at lower fees that traditional collection vendors.

Annualized Recoveries
Result = 38% Increase in Recoveries

Credit Balance & Overpayment Collections
TREND’s modules analyze insurance paid claims data, COB primacy & transactional data to produce optimal outcomes for our customers
Analysis and Recovery
TREND obtains system access and reports from Providers to identify, analyze and recover client overpayments on accounts residing in a credit balance state.
Seamless Integration and Resolution
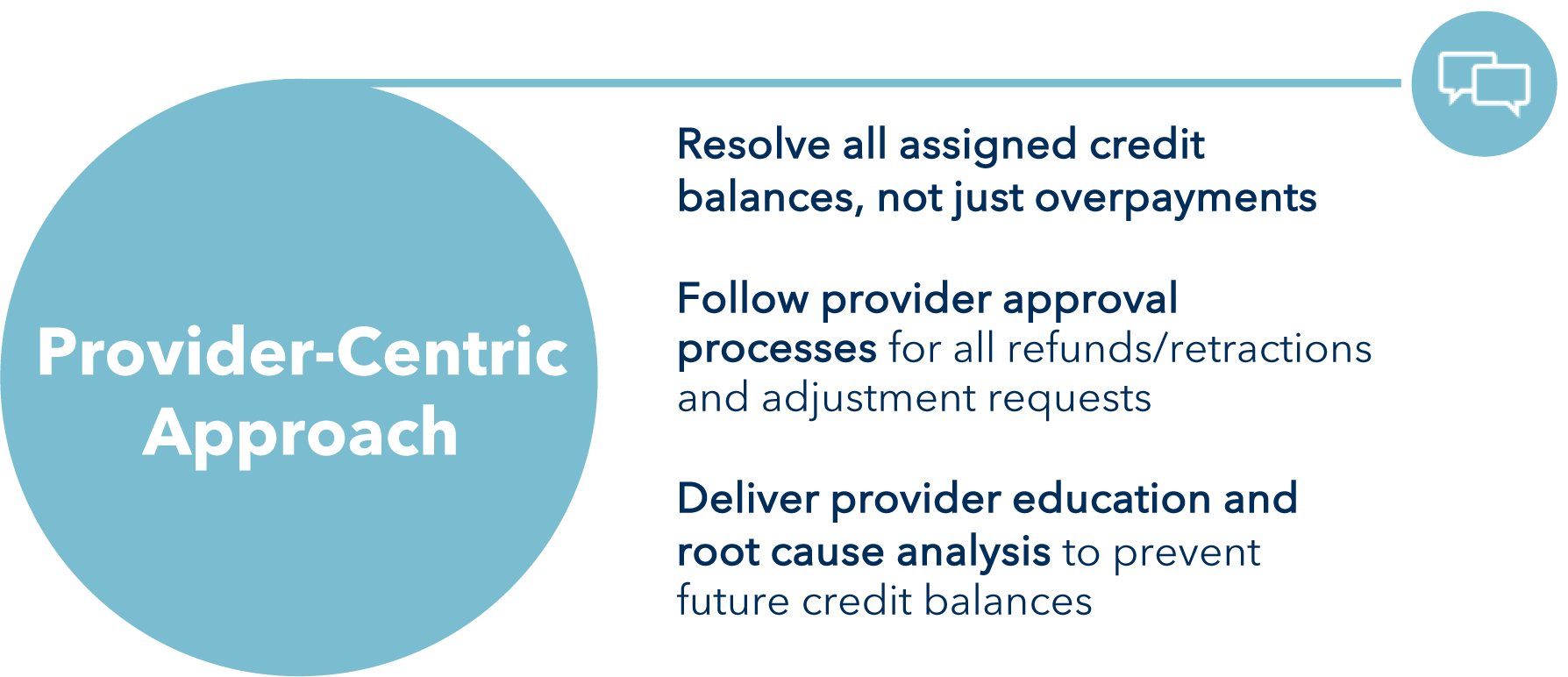
We provide resolution to all assigned credit balances, not just refunds, following existing Provider workflows.
Technology-Enabled Solutions
TREND’s comprehensive, technology-enabled solutions and robust reporting allows for deep root cause analysis to help prevent future overpayments.
Getting started with Overpayment Collections
Direct Interactions and Expedited Collections
TREND reviews, validates and interacts directly with Provider on the Payer's overpayment inventories that require approval for retraction or check recovery. TREND’S provider access and relationships expedite collections for our clients.
On-site Support = Faster Collection
On-site representative reduces provider abrasion and helps create efficiency for Payer and Provider! Faster collection turnaround vs. standard mail/telephone collection process at lower fees that traditional collection vendors.
Get better results, new concepts, automated intelligence

Payment Accuracy
CASE STUDY
Payment Accuracy

Plan Overview
Single-state BCBS Plan
Number of Members: ~3 Million Lives

Key Value Drivers
6 months in production
Health plan finds TREND’s workflow/reporting easy to use
Claims go from identified to retracted savings in 9 days
Reduced the health plans’ time to support by 45%
65% increase in Gross Recoveries
320% increase in average claim recovery
98% accuracy rates achieved

Annualized Recoveries

PAYMENT ACCURACY
TREND’s comprehensive and integrated Payment Accuracy solution + PrecisionGx’s leading AI Engine
More Recoveries, Faster to Results
- +16% recoveries in one month
- +65% recoveries in 2nd pass, +27% in 3rd pass in six months
- 98% human accuracy rate, 96% AI accuracy in automations
AI Built for Payment Accuracy
-
>80% automation in areas of interest for insourcing/prepay
-
~30% reduction in reliance on vendors in COB
-
AI audits 26x faster, 97% reduction in cost where automated
Getting started with our AI powered Data Mining or with Payment Accuracy Intelligence only
Bring us in for Data Mining
- Add net new recoveries within months, early or late pass
- Identify new concepts, content across claim types, lines of business
- Add the benefits of Payment Accuracy Intelligence below
Start with Payment Accuracy Intelligence only
- Get case hits with AI scoring and/or full AI audit results
- Uncover new content/concepts, underserviced areas
- Discover automation opportunities for admin. savings and better internal performance
Get better results, new concepts, automated intelligence

Membership Integrity

Membership Integrity
Accurately identify members with unknown Medicare coverage whether or not they have claims.
Break Out of Traditional COB
- Avoid vendors holding on to coverage changes until large claims come in
- Minimize reliance on COB vendors overall
- Reduce fees
- Prevent future COB
- Eliminate abrasion associated with post-pay COB
Getting started with Membership Integrity on its own or add COB Data Mining support
Membership Integrity
- Use typical claims data feed from plan
- Receive identified Medicare members with direct CMS information
- Pass to internal team to update, validate recoveries and generate results
Add to COB Data Mining
-
Add validation, primacy determination, and COB services to generate recoveries.
-
Add to existing Data Mining implementation seamlessly
Get better results, new concepts, automated intelligence

Payer Operations Intelligence

Payer Operations Intelligence
Monitor payer claims operations to detect anomalies early and automate processes
Receive a regular file to detect potential issues
- Analytics and anomaly detection covering:
- Auto-adjudication rate,
- Pending/Suspensions, Claim/$ volume, Denial rate, Utilization, Close time
- Finding needles in the haystack in real-time,
- Analyzes across claims, providers, members
Payment accuracy and operational impacts
- >80% automation potential for suspensions modeled
- +5% auto-adjudication impact
- Modeling trillions of potential patterns per week to identify:
- 25-50 top level findings (NPIs, Members, Claim patterns)
- Support payer teams to address, automate
- Add to existing Data Mining or Membership Integrity implementation seamlessly
Get better results, new concepts, automated intelligence
TREND’s modules analyze insurance paid claims data, COB primacy & transactional data to produce optimal outcomes for our customers
TREND accurately & efficiently resolves overpayments and credit balances
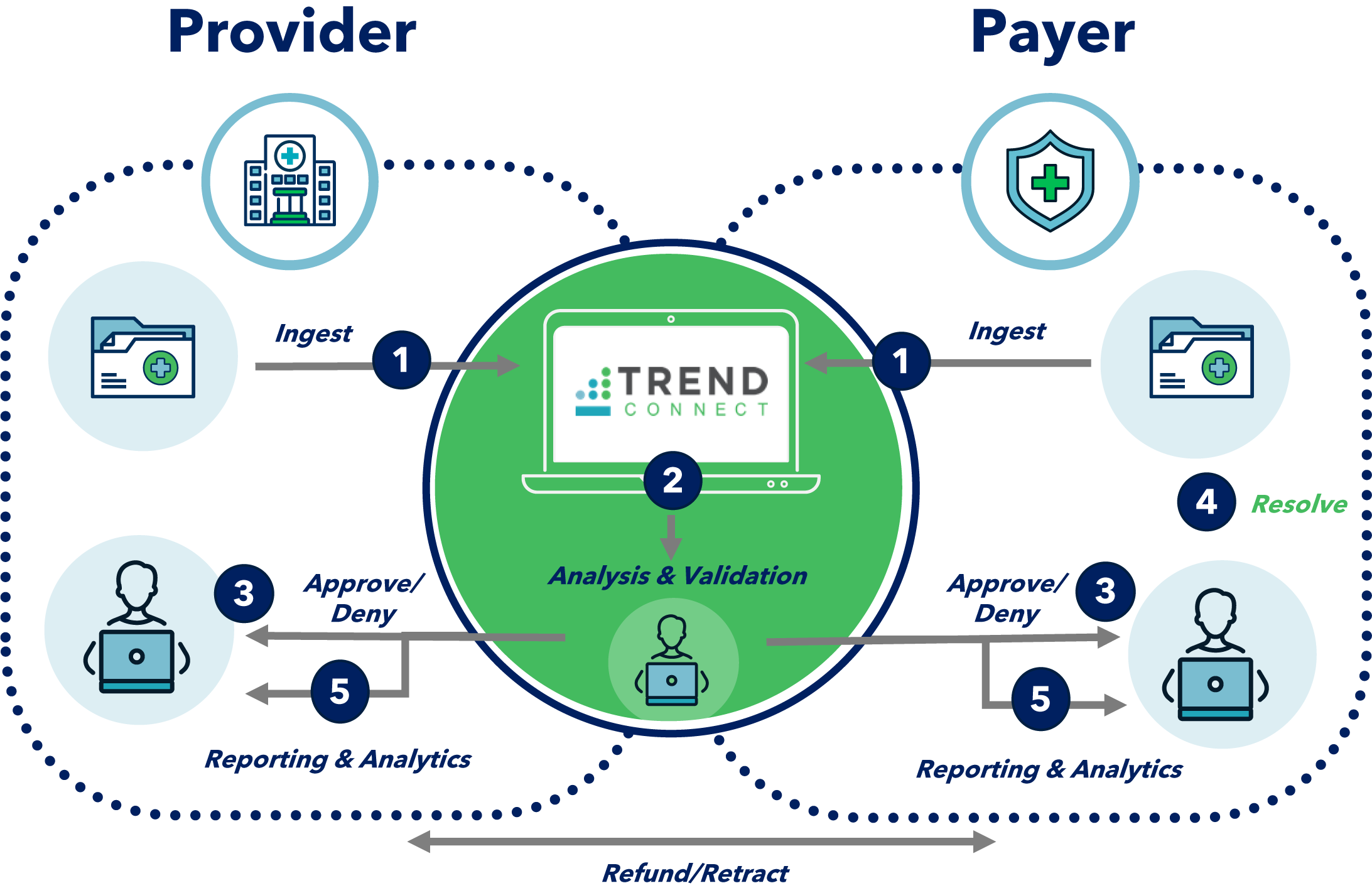
Seamless Workflow
Ingest Data
Analyze & Validate
Approve/Deny
Resolve & Correct
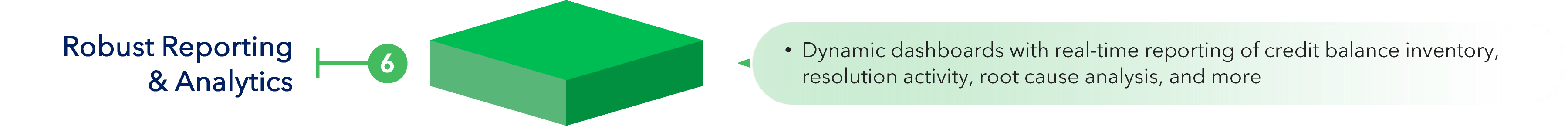
Reporting & Analytics
TREND Technologies

TRENDSubmit
Providers report overpayments through portal directly to Payer (or TREND). Target audience is non-compliant Providers, rural facilities, Physician Groups, etc. User friendly portal which provides real-time updates and reporting to Payers and Providers at no cost.

RADAR
As an extension of Credit Balance, analytics are applied to all member claims (utilizing Payer Data) as a “patient history sweep” based on target credit balance root causes to identify additional overpayment opportunity at other Providers.
AstriaChat™
The first generative AI trained to automate health insurance claims processing, audit, and recovery. To prevent and recover the more than $300B in inaccurate healthcare payments paid annually in the U.S.

TREND Technologies
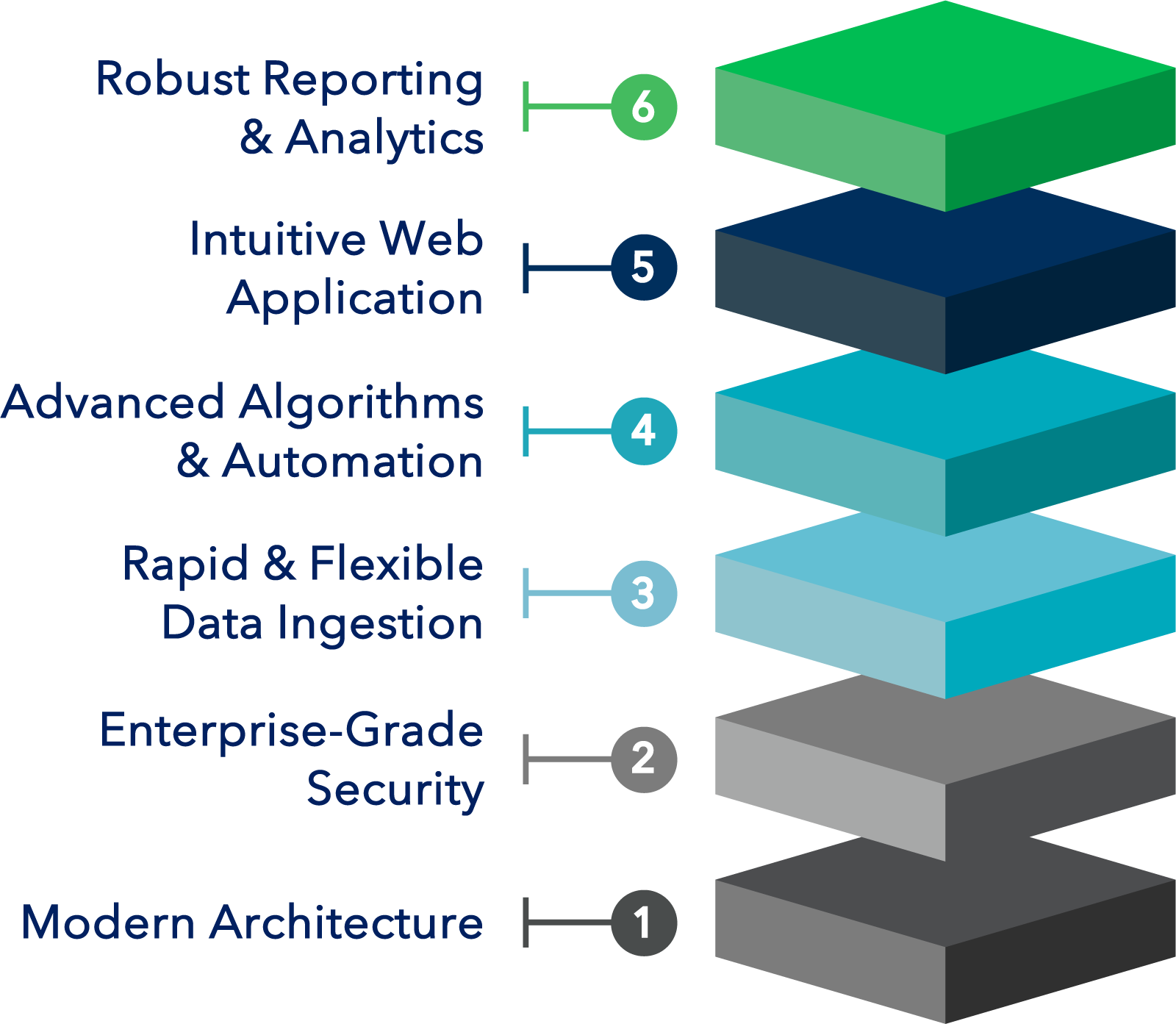
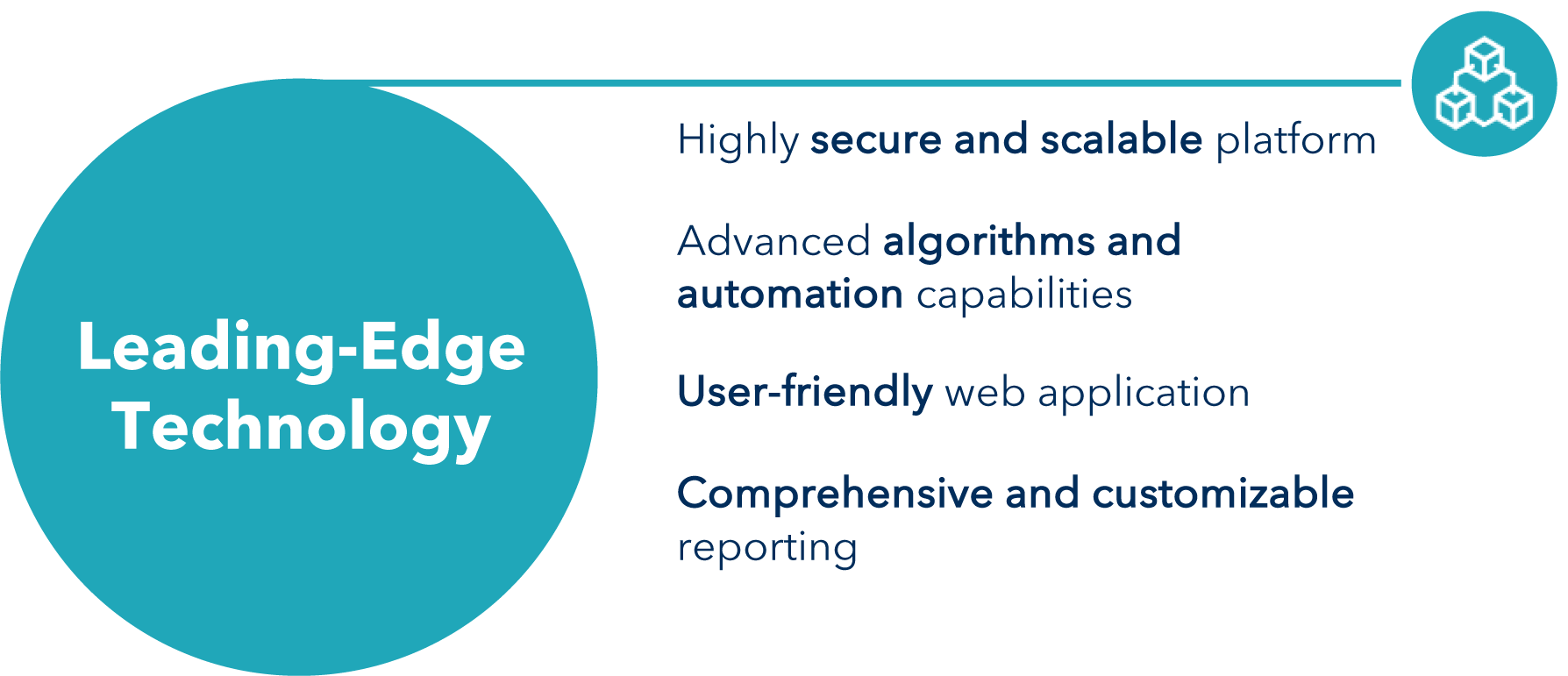
TRENDConnect is built with leading-edge technologies which enable high scalability, security and usability
The TREND Difference


TREND serves as a trusted partner to providers and payers to improve payment accuracy and reduce administrative costs for all parties

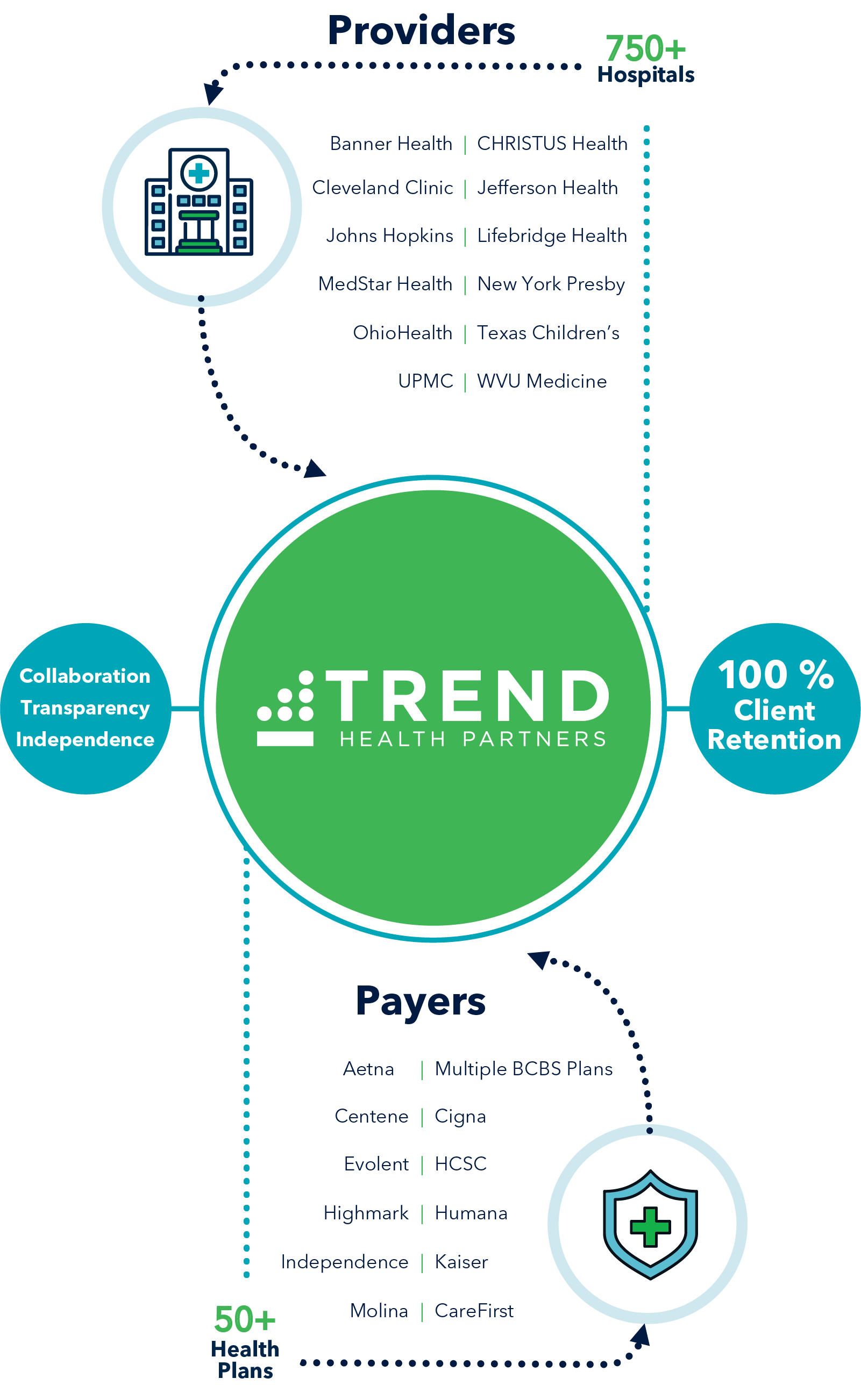
TREND operates as an extension of the provider’s business office, leveraging TRENDConnect to accurately & efficiently resolve credit balances
TREND Suite of Services
An expansive Array of Tech-enabled Services Driving Significant Value to Payers and Providers

PAYER SOLUTIONS
More recoveries, faster results
Increased payment accuracy
Detect anomalies early and automate processes

PROVIDER SOLUTIONS
Reduce costs and/or reallocate staff
Increase net revenue
Improve contract compliance
Payer #1
Multi-State BCBS Plan Multi-Service
“I love TREND’s portal. It is super easy and friendly and has all the information I ever need. I have never had an issue with them. They are very responsive to our questions, produce any information we are looking for, and they are very thorough.”
Payer #2
Multi-State BCBS Plan
Credit Balance
Payer #3
Single-State BCBS Plan payment Accuracy
Have a specific question?
Connect with us
SALES
For general questions and all other business inquiries:
MARKETING
CLIENT SUPPORT
For clients in need of customer support, please contact support:
