When Payers and Providers play on the same team, Healthcare gets better.
We’re healing adversarial payer-provider relationships with collaborative solutions that benefit all parties and make healthcare more efficient.

Welcome to a new era of alignment in Healthcare
#1 Best in KLAS for both Payers and Providers,
proving collaboration can outperform conflict.

Trusted by 1,000+ Hospitals & 100+ Health Plans
The adversarial payer-provider dynamic is costing healthcare billions, and leaving patients in the wake.
It’s time to start a new TREND.
r
e
n
D
It’s better when we play together.
The Old Way
Historically, healthcare payers and providers have been at odds – playing an endless game of tug of war for who’s owed what. This friction not only makes payer and providers’ jobs harder, it damages the patient experience and drives up healthcare costs.

Providers struggle to…
- Keep up with credits
- Avoid denials
- Get paid correctly
Payers struggle to…
- Prevent overpayments
- Control/reduce costs
- Minimize waste
The TREND Way
With TREND, payers and providers collaborate to optimize the reimbursement cycle and usher in a new era of healthcare efficiency.
Ensure accurate payments
Minimize denials
Prevent credit balances/overpayments

We're creating...

Payers & Providers Need A Neutral Party to Get Payments Right and Prevent Back-End Conflict
You can avoid the battle on the back-end by getting it right on the front-end.
As a truly independent entity, TREND advocates for neutrality and rejects the outdated adversarial model in favor of building collaborative solutions.
We're Independent
We're Unbiased
Solutions
We’re Solving Problems, Not Transferring Blame
Our core solutions bring payers and providers together to solve some of the most pervasive challenges
in healthcare financial management.
Payment Integrity
Get payments right the first time with AI-enabled technology.
Denial Management
Minimize the impact of denials through payer-provider collaboration.
Credit Balance
Credit Balance
Denial Management
Minimize the impact of denials through payer-provider collaboration.
Payment Integrity
Get payments right the first time with AI-enabled technology.

TREND HEALTH PARTNERS
Payer-Provider Collaboration Manifesto
Discover why we believe payer-provider collaboration is the only way to heal the healthcare system.
DOWNLOAD OUR LATEST EBOOK
Transforming Medical Record Review with Artificial Intelligence
Learn how AI is disrupting this industry and how to harness this technology to increase the efficiency and ROI of the review process.
Increasing the efficiency of the medical record review process has traditionally focused on increasing the speed of traditional medical record reviews..
Technology
Introducing TREND Connect™
TREND Connect is the unified platform that enables true collaboration between providers and payers.
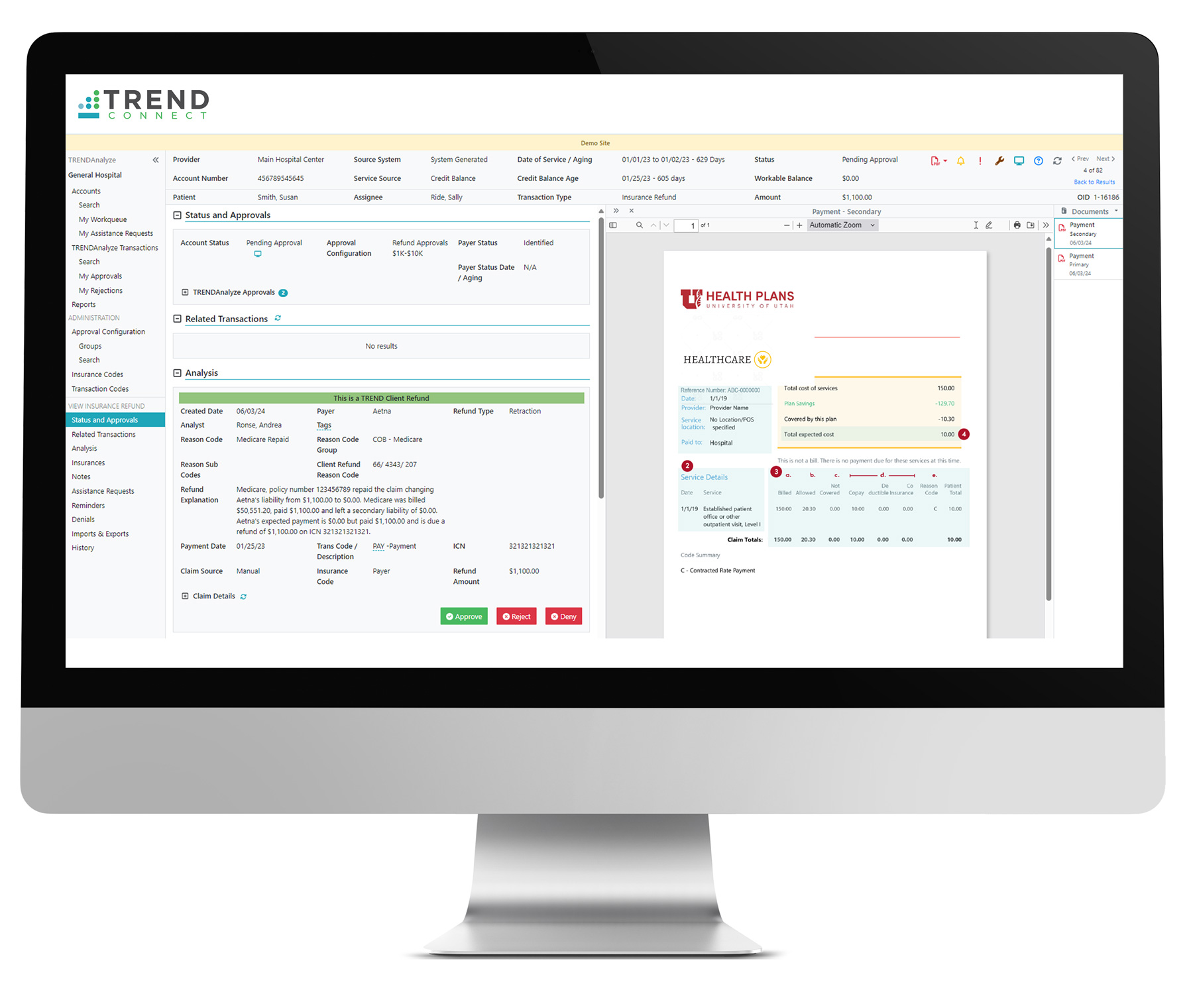
Taking Healthcare From Silos to Synergy
With TREND Connect, payers and providers are brought together on one platform; creating a mutual view to resolve claim issues together.
✔ Validate Overpayments, Resolve credit balances in medical billing
✔ Reduce Denials with our denial management solutions
✔ Discover Mutually Beneficial Opportunities
Get Payments Right, Avoid the Fight
By getting payments right on the front-end, you avoid conflict on the back-end. Root cause insights provided by TREND Connect help prevent incorrect payments and make healthcare more efficient for all. This is true Payment Integrity.
Powering Industry Experts With AI-Enabled Tech
With access to powerful tools like CAVO® in the TREND Connect platform, payers and providers can supercharge their teams by accelerating medical record review and so much more.
The Result
With TREND, Everyone Wins
By shifting the industry’s paradigm from competing to co-creating, and harnessing the collective strength of our teams, meaningful change will finally happen; improving outcomes for all parties.

Payers Benefit
Improved Payment Accuracy
Increased Staff Efficiency
Cost Reduction

Providers Benefit
Improved Financial Performance
Reduced Administrative Burden
Improved Payer Relations


