Are you tired of the fight?
Unlock the power of collaboration
WITH

A new, cooperative dynamic between payers and providers.

TREND’s collaborative approach yields tremendous benefits to both payers and providers
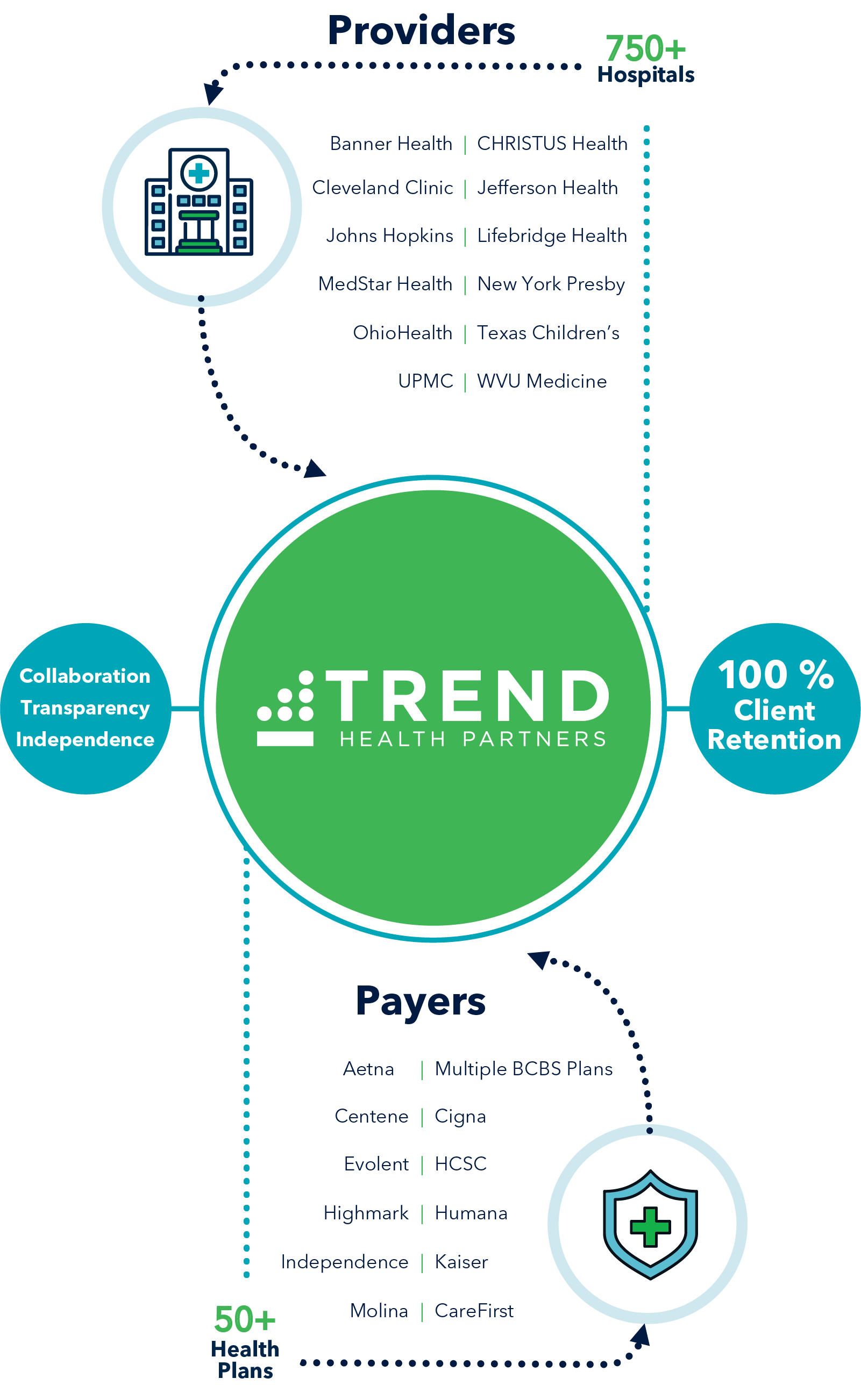
+ Hospitals
+ Health plans
TREND has processed
Million Credit Balances
TREND has identified
Recoveries
Million in Overpayments
Offloading the equivalent of
FTE 's worth of work from providers
Which could generate
Million in Additional Collections
TREND serves as a trusted partner to providers and payers to improve payment accuracy and reduce administrative costs for all parties
Solving Provider Challenges
Solving Payer Challenges

TREND operates as an extension of the provider’s business office, leveraging TRENDConnect to accurately & efficiently resolve credit balances
TREND Suite of Services
An expansive Array of Tech-enabled Services Driving Significant Value to Payers and Providers

PAYER SOLUTIONS
More recoveries, faster results
Increased payment accuracy
Detect anomalies early and automate processes

PROVIDER SOLUTIONS
Reduce costs and/or reallocate staff
Increase net revenue
Improve contract compliance
TREND is compatible with
MEDITECH
ALLSCRIPTS
EPIC
CERNER
Payer #1
Multi-State BCBS Plan Multi-Service
“I love TREND’s portal. It is super easy and friendly and has all the information I ever need. I have never had an issue with them. They are very responsive to our questions, produce any information we are looking for, and they are very thorough.”
Provider #2
20 Hospitals
$4B NPR
“TREND is kind of an extension of my team, so what we expect from my team we expect from them… They respond very timely to any question with reports, claim issues, what is the status of an account – their communication is probably one of the best I have seen.”
Payer #3
Single-State BCBS Plan payment Accuracy
“Vendors put on a pony show, and integration with a payer is always a challenge, but not so with TREND–their systems, their workflows, their reporting tools all did what they said, and it was a seamless integration with our process.”
Answers to Your Questions
What are credit balances?
It is a common misconception that a credit balance is evidence of an overpayment or an indication that someone is owed money back. A healthcare credit balance is more appropriately defined as payments and contractual allowances exceeding total charges within the financial accounting system.
Do all credit balances result in overpayments?
According to the Healthcare Financial Management Association (HFMA), approximately 75% to 80% of credit balances are the result of misposted allowances, charge credits subsequent to billing and incorrect collections at the time of service. Only 20% to 25% of credit balances actually prove to be overpayments due to be refunded to an insurance payer or the patient.
Why do providers use credit balance vendors?
The average teaching hospital manages well over 50,000 credit balances annually. For the average multi-site health system, that number increases by a multiple of 10. The annual cost associated with the effective management and resolution of credit balances by the average hospital system is between $1.5 and $2.5 million. Progressive hospitals and health systems are working with companies like TREND. TREND provides technology and support services to reduce their costs by between 30-40% to allow their organization to re-deploy their financial staff to more valuable revenue generating activities.
What do you mean by Payment Accuracy?
According to CMS, more than $170 billion in claims are paid in error every year due to the complexity of our healthcare delivery systems. This is equivalent to more than 7% leakage coming from the commercial market and 10% from the governmental market. TREND deploys an advanced technology platform and proven claims data modeling techniques to drive the identification, validation and resolution of payment errors at scale.
What does collaboration mean between payers and providers?
TREND employs operational and technical experts from payment integrity and revenue cycle industries. Many of the claims that are paid in error exist due to a breakdown in communication between payers and providers. TREND has developed excellent relationships with payers and providers to facilitate a transparent and collaborative connection. We are seeking to bridge the gap in that breakdown as it relates to overpayment recoveries. We take a deeper dive into the root cause of the overpayment and provide education or recommendations for claim edit fixes to efficiently and accurately resolve current overpayments in addition to preventing any overpayments from occurring in the future.
Have a specific question?
Connect with us
SALES
For general questions and all other business inquiries:
MARKETING
For marketing, media/press inquiries, events, and sponsorships:
CLIENT SUPPORT
For clients in need of customer support, please contact support: